Noncommunicable diseases like cancer often require prolonged management and sometimes, hospitalization and recovery, entailing huge expenses that can push patients and their family to financial hardship, even poverty.
People who seek cancer care hit barriers at every turn. Income, education, geographical location and discrimination based on ethnicity, race, gender, sexual orientation, age, disability and lifestyle are just some of the factors that can negatively affect care.
The most disadvantaged groups are also more likely to have increased exposure to a host of other risk factors such as tobacco, unhealthy diet or environmental hazards. In fact, the World Health Organization (WHO) said about a third of deaths from cancer are due to tobacco use, high body mass index, alcohol consumption, low fruit and vegetable intake and lack of physical activity.
Every year on Feb. 4, we observe World Cancer Day. The cancer community comes together, through capacity building and advocacy initiatives, to intensify the call to reduce the global cancer burden, promote greater equity and integrate cancer control in the world health and development agenda.
The theme of this year’s celebration is “Close the Care Gap.” The more we know about cancer, the more lives we can save. However, the reality today is that the world’s population lacks access to the full range of essential health services. This is the equity gap, and it is costing lives.
If we do not take action, cancer will continue to be a leading cause of death worldwide. There were almost 10 million cancers death in 2020, or about one of six deaths, according to the WHO. Globally, the most common cancers are breast, lung, colon and rectum and prostate cancers.
Meanwhile, human papillomavirus and hepatitis are responsible for about 30% of cancer cases in low and lower middle-income countries.
The Department of Health (DoH) said cancer is among the top three leading causes of death in the Philippines, and its burden is increasing. For breast and lung cancer alone, cases increased annually by 5.9% and 7.2%, respectively, between 2012 and 2018, according to a Philippine Institute for Development Studies (PIDS) report.
The most common types of cancer in the Philippines are breast, lung, colorectal, liver, prostate and cervix uteri, with the highest share of deaths from lung, liver, and breast cancers, according to PIDS.
Patient organizations have noted that many don’t consult their doctors regularly, making it more difficult to prevent, detect and treat cancer. Some may think of a cancer diagnosis as a death sentence. But the WHO said between 30% and 50% of cancers can be prevented by avoiding risk factors and implementing evidence-based prevention strategies.
One can lower the risk of getting many common cancers by making healthy choices, the US Centers for Disease Control and Prevention (CDC) said. Advancements in science, including those related to innovations in diagnostics, vaccines and medicines, allow for many cancers to be cured if detected early and treated effectively.
The CDC said screening tests can find some cancers early, when treatment works best. Meanwhile, vaccines can help prevent several kinds of cancer. For example, the human papillomavirus vaccine helps prevent most cervical cancers and several other types of cancer. The hepatitis B vaccine can help lower the risk of liver cancer.
A new era of innovation is also pushing the frontiers of science and having a significant impact on the lives of patients with a wide range of cancers, noted the Pharmaceutical Research and Manufacturers of America. It said new cancer medicines have led to treatment advances in recent years, preventing deaths across many tumor types, particularly for breast and lung cancers and melanoma.
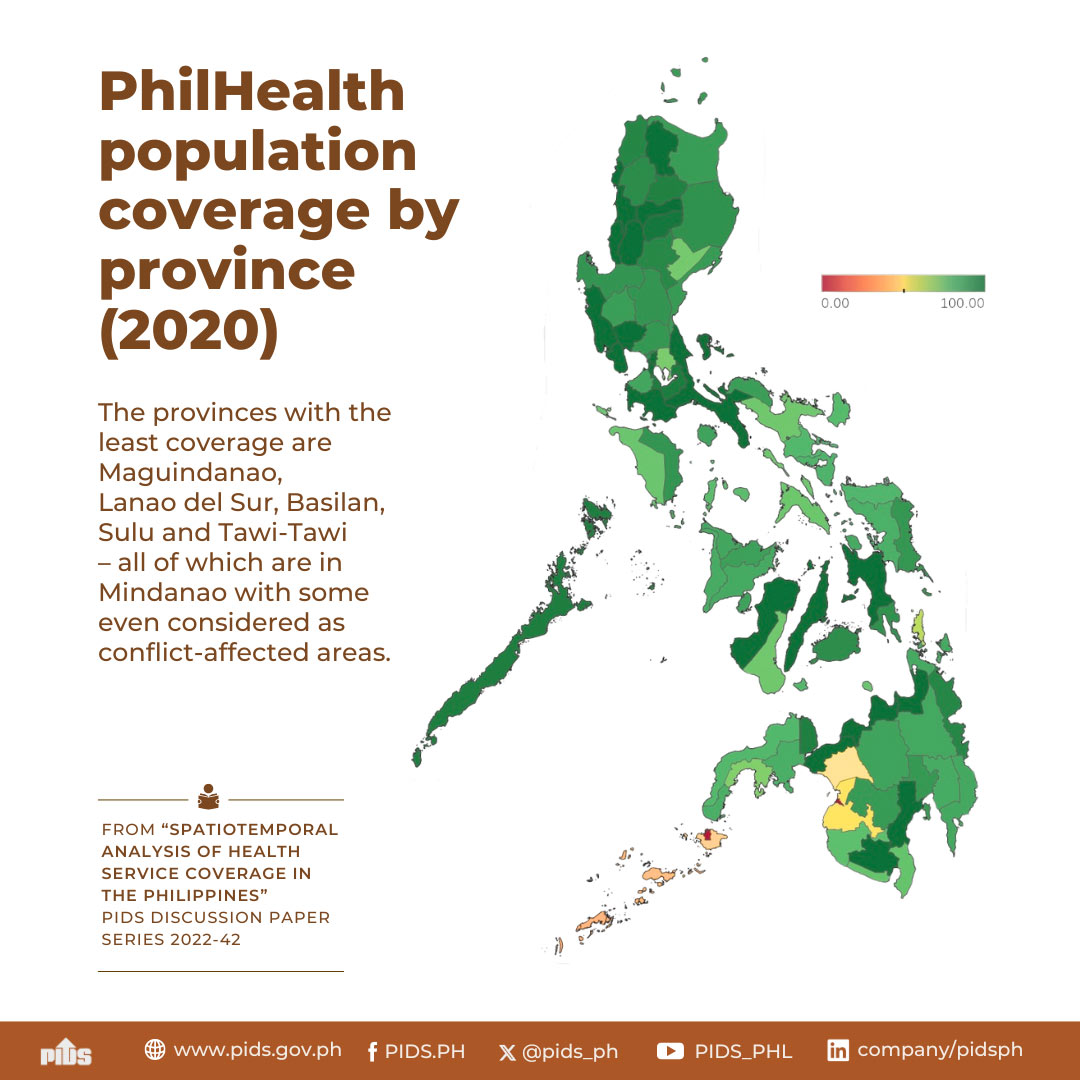
Some patients also do not seek or continue their treatment due to the anxiety of putting a heavy financial burden on the family. While the passage of the Universal Health Care (UHC) Act and National Integrated Cancer Control Act (NICCA) can ensure equitable and rational delivery and financing of the cancer care continuum, the full implementation of these laws has been delayed due to challenges posed by the COVID-19 pandemic. Patients who pay for their own treatment are often unable to continue with treatment and care.
Leveraging on the NICCA and UHC Act implementation to put cancer prevention and care on the national agenda will be crucial to achieve health equity. The Health department, PhilHealth and private sector can use these landmark laws as motivation to increase overall cancer care financing. Continuous engagement of the Executive branch and private sector with legislators can ensure that the NICCA is progressing as envisioned, according to the PIDS paper.